If trends continue, North Carolina hospitals are expected to set a milestone this Wednesday when the number of patients hospitalized with COVID-19 is predicted to reach the highest point during the pandemic. At the same time, hospitals are reporting record staff absences, causing health care centers to again delay non-urgent procedures, and prompting renewed concerns about hospital capacity.
The double hit of a surge in patients but fewer workers has already caused hospitals across the state to throttle back on non-urgent cases to reserve resources for patients with severe COVID-19 symptoms. The main constraint to hospital capacity is not the physical bed, or square feet in a hospital building – it’s staffing, particularly nurse staffing. Already, North Carolina – and the country – is in the middle of nurse burnout, threatening the health care system's ability to care for COVID-19 patients. The omicron surge has only compounded that threat.
On Tuesday, N.C. Department of Health and Human Services reported 3,991 people hospitalized with COVID-19. That’s just one patient shy of the all-time record, set January 13, 2021, with 3,992 patients. Over the past two weeks, hospitals have admitted nearly 450 patients per day, another pandemic all-time high.

At the end of last week, UNC Health Care reported more than 1,000 workers with required absences due to either testing positive for COVID-19, or because of a close contact with someone who tested positive. At Duke, that number was more than 890 (the Duke figure includes university staff, though a spokeswoman said the "majority" were at Duke Health). At WakeMed, there were more than 250 absences. At all hospitals, these absences surpassed those from previous waves.
So far, most hospitals have been able to balance worker and patient scheduling. DHHS data estimate there are still close to 4,000 beds available in North Carolina, though capacity isn't spread evenly across the state. Some of this capacity is created by hospitals delaying other kinds of care, and rescheduling some procedures. Although classified as non-urgent, these procedures often feel important to those patients who have to wait until this surge recedes to reschedule.
Hospitals across the state report total capacity of about 20,000 inpatient beds, 2,200 ICU beds, and 3,700 ventilators.

Omicron surge impacts differently than Delta
This current omicron surge has impacted the health of North Carolinians differently than previous COVID-19 waves; both in advantageous and negative ways. The omicron coronavirus variant is far more transmissible, but it seems to be less severe. More treatments are available, and more people are vaccinated now than in previous surges. Although hospitals are short-staffed, they have a better understanding of how to provide care, and are able to keep a larger percentage of patients out of the most intensive care settings.
More than two-thirds of everyone in North Carolina ages 12 and older have received two doses of the vaccine, and nearly 2.7 million people in the state have received the additional booster shot. These people are protected against the worst symptoms even if they contract the virus and become a breakthrough case.
Since the beginning of the pandemic, there have been close to 1.9 million positive tests collected by the state, and close to 20,000 people have died from COVID-19. All these cases have given the health care system and its workers an education on how to treat patients. New treatment options are available, though supplies are limited, and hospitals have rationed these treatments for only the most at-risk patients.
"We've learned a lot about COVID. So the patients that may have been in ICU at the beginning of this pandemic are now maybe not in ICU," says Dr. Adia Ross, the Duke Regional Hospital chief medical officer. "But that doesn't mean that they're not ill. It just means that we have developed systems to take care of them."
On Tuesday, hospitals reported 722 Intensive Care Unit beds with COVID-19 patients. The record number of patients in ICU beds was set September 13, with 955 patients in ICU. At the height of the first hospitalization wave, the record of patients in ICU beds was 880, a mark set on January 15, 2021.
The percentage of COVID-19 patients in ICU dropped to 18.1% Monday, the lowest rate since DHHS began reporting the metric at the beginning of summer 2020. Ross says a higher vaccination rate, and better treatment options and strategies likely contribute to this lower rate. But health officials stress that regular hospital floor level care is still severe, and the omicron variant is also deadly.
"We have people sick in the hospitals – right now – with omicron, who are on ventilators," says Dr. David Wohl, an infectious disease specialist with UNC Health Care. "So we should not be fooled or lulled into some sense of security. This could be a very dangerous virus for a lot of people, especially if they're un-vaccinated."
Hospital workers fear that even though a smaller percentage of people will require hospitalization, that because so many people will contract the highly contagious virus, the total number of patients could still pack hospitals full.
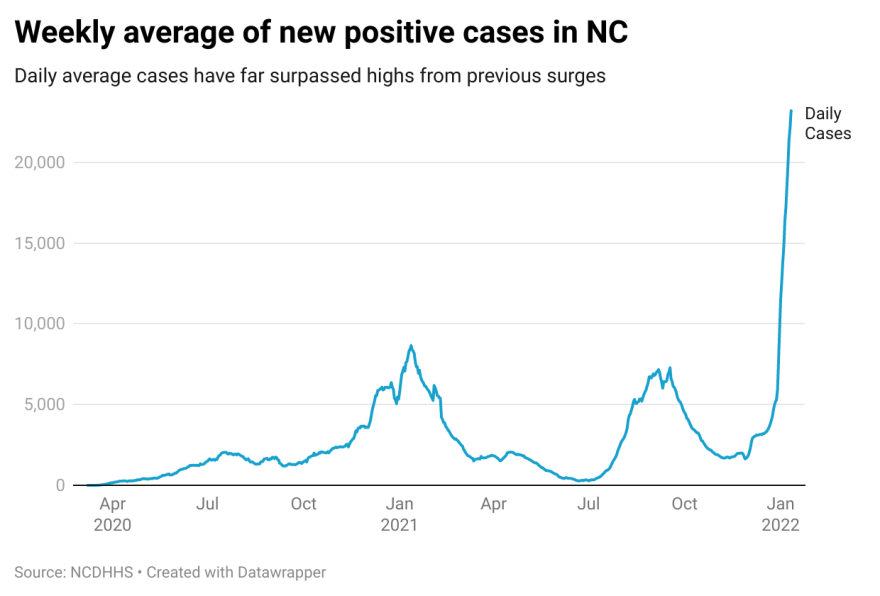
On Monday, DHHS reported a seven-day rolling average of more than 22,000 new positive cases per day. That's more than double the number of daily cases from previous waves. In January of last year, the seven-day average of new cases never surpassed 8,700 cases per day. During the delta wave, the seven-day average never surpassed 7,300 cases per day.
That means that even if half of those infected with the omicron variant required hospitalization compared with previous variants, it would still lead to more total hospitalizations across the state.
"Unfortunately, there is still a critical mass of people who are vulnerable to getting very sick from COVID-19, even with omicron. And as long as that critical mass of people remains substantial, we will have all these mitigation strategies – the masking, the boosting – because we're doing this all to build a moat around those vulnerable people," says Wohl. "And it's those vulnerable people, the majority of which are the unvaccinated, that is really the engine for everything that's affecting our society right now when it comes to COVID-19."

‘Incidental’ cases are still patients with COVID-19
Because the omicron variant has spread so fast, some patients come to the hospital for reasons other than COVID-19, only to test positive for the virus once admitted. Hospitals call these "incidental" COVID-19 patients. While these patients might appear to distort COVID-19 hospitalization figures, health leaders say hospitals need to treat these patients just like any patient who comes to the hospital with COVID-19 as the primary reason. These patients must be sectioned off from other patients in order to prevent spreading the virus, and hospital staff must take extra precautions when providing care, which takes additional time and resources.
"It's also important to note that it is not always clear what role COVID may or may not play in someone needing hospitalization,"Catie Armstrong, a DHHS spokeswoman, wrote in an email. "For example, COVID can worsen other health conditions (heart conditions, breathing issues, etc.) and lead to hospitalizations that may not have been necessary without COVID-19 playing a role."As omicron sweeps through the state, medical leaders are keeping close watch on this intersection of cases, beds and burnout, and continuing to raise the alarm over pressures on the health care system as a whole.





