The U.S. Supreme Court appears set to overturn the landmark Roe v. Wade decision that gave American women access to legal abortions.
Since then, there has been a lot of discussion about the political fallout, the leaked opinion, protests, and more. WUNC Health Reporter Jason deBruyn spoke with Dr. Beverly Gray, founder of the Duke Reproductive Health Equity and Advocacy Mobilization team, and Dr. Jonas Swartz, assistant professor of Obstetrics and Gynecology, about the impacts on women's health if Roe is overturned.
Answers have been edited for clarity and length.
Jason: What was your initial reaction when you first saw the draft opinion?
Gray: Unfortunately, I wasn't too surprised. I think a lot of us in the family planning community were expecting this type of news. We just didn't know exactly when it was going to happen. And it's still unclear what the final ramifications will be once a final decision is made. But we're clearly very worried, anxious for our patients and what opportunities will be available for them.
I wonder if maybe there's a silver lining here in North Carolina. I think from your perspective, North Carolina isn't where you would want it to be, but it's in a better position than other states, particularly in the South. Already 17% of abortions in North Carolina are from out-of-state patients, according to the Centers for Disease Control and Prevention, so maybe North Carolina can be a place of safety for patients from surrounding states?
Swartz: I know that we have already seen an influx of patients who have lost access to abortion in Texas. But you worry about whether people are going to be able to travel to get abortion. Many women in North Carolina already have to travel significant distances to get abortion: 92 counties in North Carolina don't have an abortion clinic and over 50% of women of reproductive age live in those counties. So North Carolinians already have to go a long way to seek abortion in many cases.
What are the health impacts on women if Roe is overturned?
Gray: For many people in the South, they're already living a post-Roe existence. They don't have access, they live in rural areas, they have insurance that doesn't cover abortion care. Many people don't have money saved up for an emergency that costs $400 or $500. They just can't afford it.
North Carolina is a hostile state with respect to abortion law. We have a 72-hour waiting period in our state, which a lot of folks in North Carolina aren't aware of. So they call for an appointment. And our state legislators have decided that – you know what? – people who want an abortion need to go sit in the corner for 72 hours to get care. We're punishing the patients who don't have the means to seek care. We're punishing the patients who can't afford care.
We're punishing immigrants. We're punishing trans patients in that. We're already living in a situation where there are incredible disparities in care. And those will continue to worsen, especially in the South.

Let's talk a little about safety. It's reasonable to say that overturning Roe would likely lead to fewer abortions, but clearly it won't eliminate them. However, it will likely make it more dangerous for women who seek abortions. What are the effects on safety to women going to be?
Gray: Abortion bans decrease access to safe abortion. Ideally, the scenario is that patients have a supportive provider who's caring for them, who can be there to answer questions, who's not worried themselves that they're going to be prosecuted for caring for a patient.
There are some differences to how care will look like now compared to 40 years ago in a pre-Roe era, in that we have access to medication abortion which has an outstanding safety record. And so there's a lot of evidence that medication abortion can be managed safely under the care of a medical provider.
It's fair to say that medicine has advanced significantly since the 1960s, so we wouldn't expect abortion care to go back to the way it was pre-Roe, but likely less safe than when currently performed legally. Let's stay on the safety theme for a bit. How safe are legal abortions currently?
Swartz: People have two basic options for abortion. They can choose to have a medication abortion, which is accomplished through a combination of pills. In North Carolina, they have to take the first pill in the presence of a physician, and then they take the second set of pills often at home, have heavy bleeding with a miscarriage, and then return for medical care to verify that the pregnancy has passed. And medication abortion is safe up to 11 weeks of pregnancy.
Some people choose to have a surgical abortion. That's often a quick office procedure that takes 5 to 10 minutes. It can be performed with a handheld vacuum aspirator or with an electric vacuum machine. People can have a range of anesthesia for that. They can just have numbing medicine, they can have some oral sedation medication to make them more comfortable, or they can have IV sedation. They can even choose to be asleep in the operating room for those procedures.
And then abortion in the second trimester often takes place in the clinic setting or in the operating room. People usually have sedation for that. But again, it's a 5 to 15 minute procedure that's safe. People are able to go home and return to their normal lives that same day.
Gray: I think there are a lot of misperceptions around the safety of abortion. And I think there are a lot of fear tactics that anti-choice groups use to make it sound like abortion impacts fertility or abortion is super dangerous. It's one of the most common procedures performed in this country. By the time women are menopausal, one in four will have had an abortion in their life.
Because of the stigma of abortion, people just don't talk about it. By getting our voices out there about how common abortion is, how safe abortion is, hopefully people will feel more comfortable sharing their own stories. You probably have a family member that's had an abortion; you probably have a friend that's had an abortion. And if no one's ever told you that they've had an abortion, that means they don't feel safe talking to you about it. So what is it about you that makes you an unsafe set of ears?
One thing that has always occurred to me is that people talk past each other on this issue. The group that supports choice, sees a fetus as only part of a woman's body, not its own separate life. While those who support stricter regulations see a fetus as its own life, worthy of protection. Maybe address this from a medical perspective: What is a fetus, and at what point does it change from something without life, to something with life?
Swartz: I think that's an important question and a really challenging one because it gets at the base of the intersection of science and medicine and philosophy and religion. And to me, that's more of a religious question, and something that is generated from someone's religious beliefs, as opposed to something that can be definitively determined through medicine. We have freedom of religion in this country. And so there's no reason that someone else's religious beliefs should be able to make a decision about what one of my patients does with her body.
I think the more important consideration is that people have to be able to make decisions and have autonomy about what they do with their bodies. I care for patients who also have different conceptions of what sort of agency a fetus has in their life. But universally, the people that I care for have chosen abortion because that's the right decision for them and for their family at that time. And so I think getting caught up in that debate, we're often sort of missing the more important question, which is that an individual has to make the choice that's right for them or their family.
That makes sense, but that does have limits, I mean, I couldn't say that my five-week-old child isn't a human yet, because my religious belief is such that I don't view that as a child yet, right? We do need to have laws to provide some guardrails against all kinds of extremism, religious included. But, of course, fundamentally that's a big part of the problem here, right?
Swartz: In most of the country, the line that you're talking about is fetal viability. So when a fetus could live on its own outside a body. Generally that line is somewhere from 23 to 24 weeks, but it actually is very individual. There are some fetuses that will never be able to live independently outside of someone's body: if they have severe anomalies, or other genetic changes. To draw some distinct line misses the fact that there's variation in terms of how fetuses develop. Yes, there are guardrails within society to keep us from extreme behavior. I think in this case, we really have to focus on the fact that people need to be able to make decisions about their bodies and have autonomy make decisions about their reproductive choices.
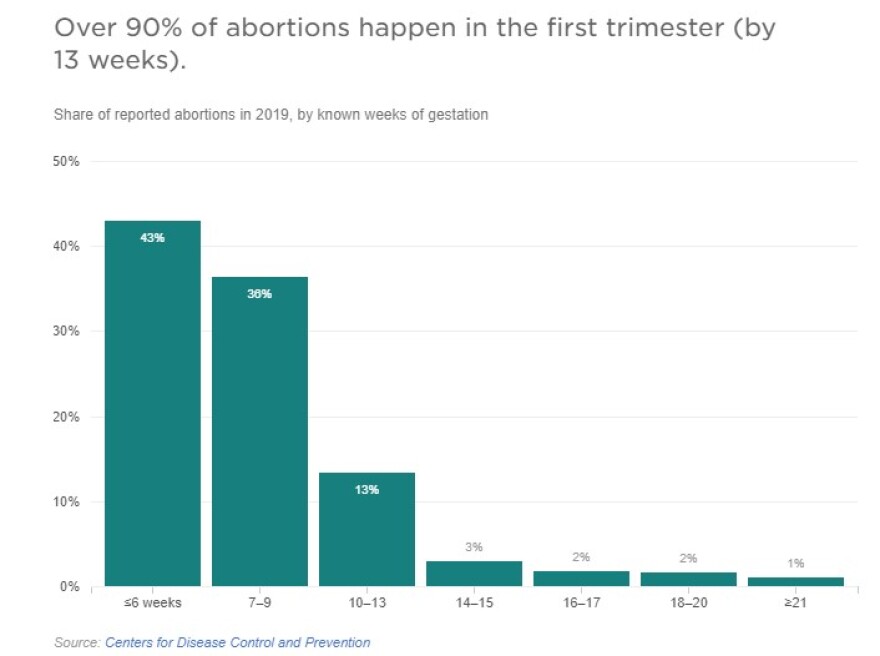
Gray: The other point to make is that the vast majority of abortion care happens in the first trimester. And we can all agree that a first trimester pregnancy is not viable outside of the body. I think there are misperceptions that there are all these third trimester abortions happening. The common, ordinary patient is seeking an abortion in the first trimester when they found out that they're pregnant.
Swartz: Another element is thinking about who gets abortion in the second trimester. Many times, we care for patients who are terminating desired pregnancies because of fetal anomalies, or genetic anomalies. And those are really difficult decisions for patients and families in difficult times for them. And it's fabulous that we are able to support them during those times. But barring access to abortion just makes it more difficult for people to access abortion when they're in those difficult situations where the life of the fetus or the mother is in question.
Building off that: Most laws that restrict abortions have exceptions for much of what you are outlining, when the life of the mother is in danger, for instance. But that can get difficult to define. Address why these exceptions, while perhaps well intentioned, have shortcomings?
Swartz: We already have to make decisions about what constitutes life endangerment. Because of North Carolina's 72-hour waiting period, sometimes there are medical emergencies that are maybe urgent, but non-emergent. Will someone lose an organ or a limb or function or critical bodily body function, if we don't wait 72 hours to do an abortion procedure? And that's a crazy choice to have to make when someone's health is at risk. When you impose more restrictions, it just puts fear in clinicians in terms of making good decisions about the medical care of their patients.
Gray: The way the North Carolina law had previously been written, there was a lot of gray area of what defines a medical emergency. Does the patient have to be in kidney failure and liver failure? That puts providers in a tough spot. And I think if abortion is further restricted, it means there are medical emergencies that happen in the second trimester, and the only way to save a patient's life is by providing safe abortion care. And so if you have trainees who are going through their residency training, and are not exposed to that care, we're looking at having a generation of providers that are just not going to have that skill set.








