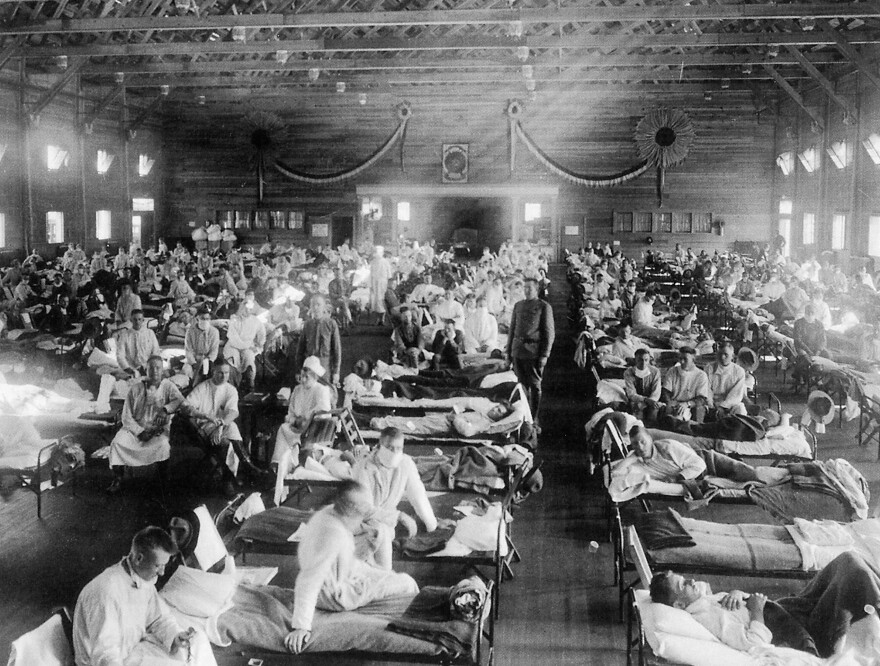
A hundred years ago, the world was struck by a nightmare scenario.
World War I was still raging. And then a suspicious disease appeared.
In the spring of 1918, the first wave of cases weren't all that bad. The death rate was low. But by November, the "mother of all flu pandemics" was spreading explosively across Asia, Europe and North America.
Known as "la grippe," the new flu strain killed quickly and at a high rate, especially among soldiers in the war. "The boys were coming in with colds and a headache, and they were dead within two or three days," a French nurse wrote on Nov. 11, 1918, the day of the armistice. "Great big handsome fellows, healthy men, just came in and died. There was no rejoicing in Lille the night of the armistice."
Studies suggest the fatality rate was 20 times that seen in previous pandemics. Up to 2 percent of the people infected died. In the U.S., it took just five weeks to kill more than 500,000 people. By summer of 1919, a third of the world's population had been infected and at least 40 million people had died. By this point, many people had picked up immunity to the strain, and the pandemic fizzled out.
Yes, what I'm talking about is the notorious 1918 flu — the strain that went on to give rise to nearly all other influenza A strains circulating today (hence the nickname "mother").
Since the 1918 flu, modern medicine has made huge strides. It has eradicated smallpox, nearly wiped out several other childhood diseases and found cures for some cancers. And just this past year, there have been glimpses that gene therapy may help with some genetic disorders, long thought to be incurable.
But what about humanity's ability to stop a flu pandemic? Um ... well, that has changed little in the past century.
"If a virus like the 1918 flu struck again, we wouldn't be able to create a vaccine fast enough to make a big difference," says Sarah Gilbert, a virologist at Oxford University, who has been working on a universal flu vaccine for years.
"It takes six months to manufacture the first doses of a vaccine for a new strain — and that's just the first doses. It will take longer to get the first million or 10 million doses," Gilbert says.
By then the virus will have spread across six continents. "It will pretty much be across the world within a month," Gilbert exclaims. Even with antiviral drugs available and modern hygiene, computer models suggest the return of a 1918-flu strain could kill more than 100 million people worldwide. (And if you're wondering what made that strain so deadly, so are scientists.)
The bottom line is: "We're Not Ready for a Flu Pandemic,"The New York Times declared in an opinion piece earlier this year.
Now Bill Gates wants to help get us ready.
"Today we are launching a $12 million Grand Challenge, in partnership with the Page family, to accelerate the development of a universal flu vaccine," Gates announced Friday at a scientific meeting in Boston. (The Bill and Melinda Gates Foundation are funders of this blog).
Yes, it's true we already have flu vaccines. But the problem is that we have too many of them.
Each year, scientists have to guess which version of the flu will be most problematic, and then — starting from scratch — they try to create a vaccine that matches that strain perfectly. This vaccine sometimes works. And when it does, it works only for one flu season. That is why it's called a "seasonal vaccine."
Right now, the whole process takes about six months, which is way too long when you're talking about an ubercontagious, airborne virus that can spread around the globe in months.
"The 2009 H1N1 pandemic was a perfect example of how that timeline just doesn't work," says Andrew Pekosz, a flu researcher at Johns Hopkins University. "We ended up vaccinating people during or immediately after the peak of the pandemic."
So there are really two approaches to make humanity better prepared for the "big one."
1. Develop a vaccine that provides long-lasting protection against multiple forms of influenza A. Then people are protected before a pandemic begins. So this would be like the vaccines we have for many other viruses, such as polio, measles and whooping cough.
2. Figure out a faster way to produce the seasonal vaccines we already have.
Scientists have already solved the second problem. Right now, the flu vaccine is produced in eggs. But years ago, scientists worked out a way to grow the vaccine in insect cells. "The process in insect cells is much, much faster than making the vaccine in eggs," Pekosz says. "We're talking about a matter of weeks, instead of months."
"But most of the vaccine manufacturers have invested large amounts of money in the egg machinery to make the vaccine" he adds. "So there needs to be a very big capital investment for the companies to move away from eggs."
Instead of investing in ways to produce the vaccine more rapidly, the Gates Foundation is now funneling more resources toward the first strategy. "Fundamentally, we are looking for unconventional approaches that ... develop universal influenza vaccines that are ready to start clinical trials by 2021," the foundation said in a statement.
"We need a broader set of ideas," says Gates Foundation president Trevor Mundel. "We need more shots on goal."
But Gilbert questions whether this is the best use of the new funding. There are several promising universal vaccines already in development, she says, including one her team is currently testing in a large clinical trial. So the holdup isn't at the preclinical stage, she says, but further down the pipeline.
"The real bottleneck is getting these experimental vaccines into testing in humans, and that is a very expensive undertaking," Gilbert says.
For instance, Gilbert says, her team needs to demonstrate that their vaccine works in a large, late-stage trial in order for governments to approve the vaccine. "Just one of these trials cost $100 million," she says.
In other words, developing an universal flu vaccine is going to take way more than $12 million from the Gates Foundation, no matter how many more "shots on goal" that new funding provides.
Copyright 2021 NPR. To see more, visit https://www.npr.org. 9(MDAxNzg0MDExMDEyMTYyMjc1MDE3NGVmMw004))